Key Takeaways:
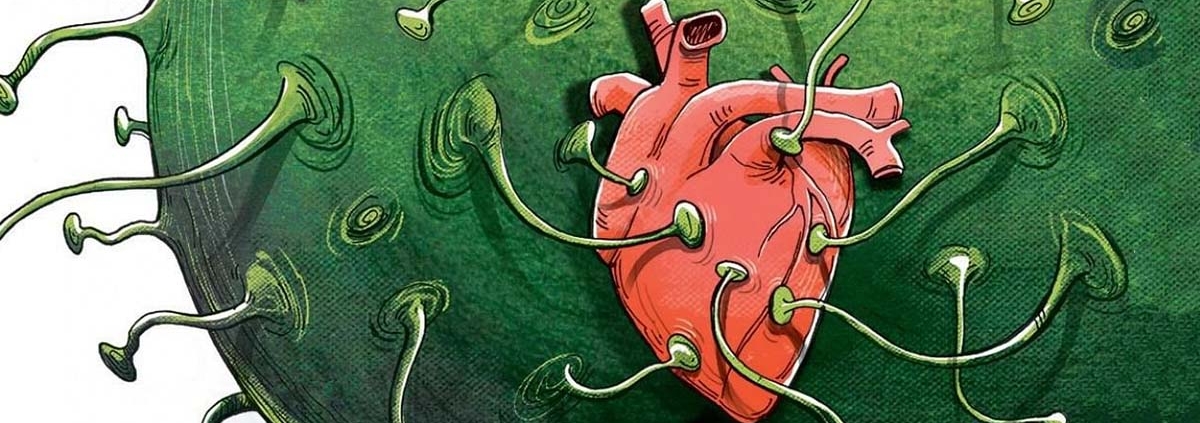
- In a study of healthy adults without COVID-19, higher brain and blood levels of various markers of inflammation were detected in participants tested after lockdowns compared with before lockdowns.
- Participants who reported greater symptoms related to mood and mental and physical fatigue had higher brain levels of one of these inflammatory markers.
New research indicates that for some individuals—even those who have steered clear of becoming infected with SARS-CoV-2—societal and lifestyle disruptions during the COVID-19 pandemic may have triggered inflammation in the brain that can affect mental health. The study, which was conducted by a team led by investigators at Massachusetts General Hospital (MGH), is published in Brain, Behavior, and Immunity.
Beyond causing a staggering number of infections and deaths, the COVID-19 pandemic has led to significant social and economic disruptions that have impacted the lives of a large swath of the world’s population in multiple ways. Also, since the start of the pandemic, the severity and prevalence of symptoms of psychological distress, fatigue, brain fog, and other conditions have increased considerably in the United States, including among people not infected with SARS-CoV-2.
To obtain a better understanding of the effects of the pandemic on brain and mental health, researchers analyzed brain imaging data, conducted behavioral tests, and collected blood samples from multiple uninfected volunteers—57 before and 15 after lockdown/stay-at-home measures were implemented to limit the pandemic’s spread.
Release date: 22 February 2022
Source: Massachusetts General Hospital