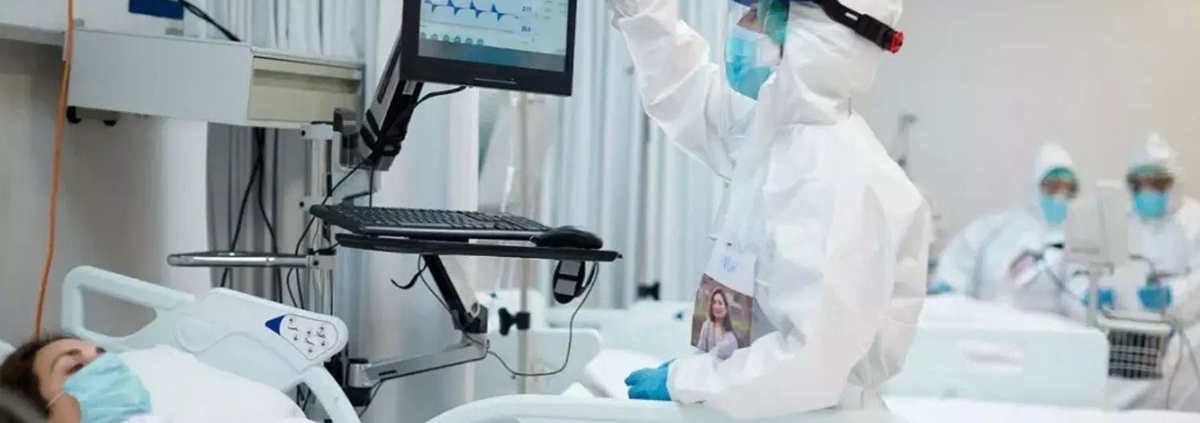
Infection-fighting B cells retain better memory of the coronavirus spike protein in University Hospital patients who recover from less-severe cases of COVID-19 than in those recovering from severe COVID-19, a new study suggests. Findings by scientists from The University of Texas Health Science Center at San Antonio were published in the journal PLOS ONE .
The study focused on memory B cells that react against the SARS-CoV-2 spike protein. Blood samples were analyzed one month after symptom onset and five months post-onset. After one month, a significant proportion of spike-specific B cells were active.
However, samples from eight individuals who recovered from less-severe disease showed increased expression of markers associated with durable B cell memory as compared to individuals who recovered from severe disease, the authors wrote. The markers include T-bet and FcRL5.
T-bet-positive, spike-specific B cells nearly disappeared from the blood samples five months post-symptom onset, the authors noted. Overall, a more dysfunctional B cell response is seen in severe disease cases, they wrote.
Release date: 23 December 2021
Source: University of Texas Health Science Center at San Antonio