Researchers from Osaka University and Kyoto University develop a stem cell-based biomaterial that can help regenerate tissue associated with low back pain and spinal issues.
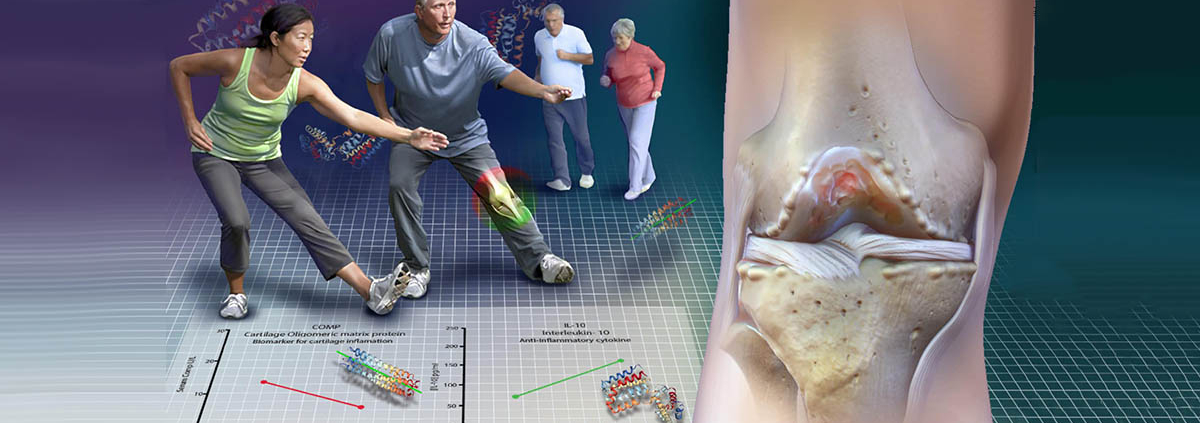
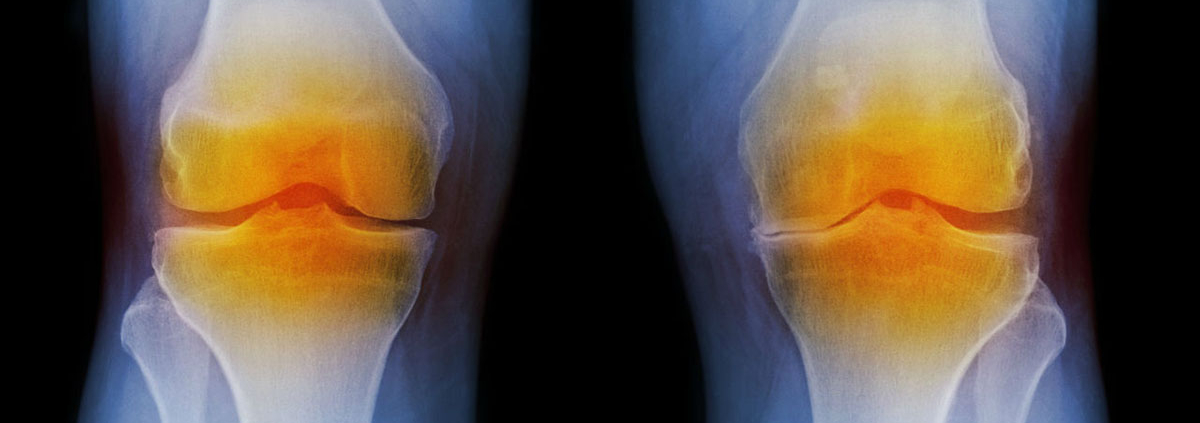
Many people have experienced the struggles of dealing with low back pain. A common cause of this pain is degeneration of intervertebral disks (IVDs), which are located between the vertebrae and help give the spinal column its flexibility. Thus, IVD degeneration can lead to more serious conditions such as spinal deformity. In a recent article published in Biomaterials, a team led by researchers at Osaka University and Kyoto University demonstrated that using cartilage tissue derived from human stem cells could help prevent the loss of functionality from IVD degeneration.
The article, “Human iPS cell-derived cartilaginous tissue spatially and functionally replaces nucleus pulposus,” was published in Biomaterials.
Release date: 15 April 2022
Source: Osaka University