Primary
Type 1: Postmenopausal (six times more common in women)
Type 2: Involutional or senile osteoporosis (twice as common in women)
Idiopathic osteoporosis: Occurs in children and young adults of both sexes with normal gonadal function.
Secondary
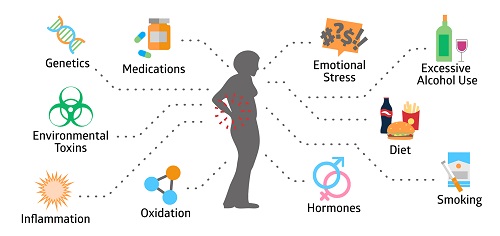
- Endocrine disorders:
- Estrogen Deficiency
- Testosterone Deficiency
- Cushing’s Syndrome (Hypercortisolism)
- Hyperparathyroidism
- Hyperthyroidism
- Gastrointestinal/Nutritional Disorders
- Vitamin D Deficiency
- Anorexia Nervosa
- Celiac Disease
- Malabsorption
- Primary Biliary Cirrhosis (PBC)
- Inflammatory Bowel Disease (IBD)
- Chronic Drug Therapy
- Anticonvulsants
- Glucocorticoids
- Genetic Disorders
- Other Conditions
- Immobilization
- Post-transplantation
- Hematologic Marrow Infiltration (e.g. Lymphoma, Multiple Myeloma)
- Connective Tissue Disease (e.g. Rheumatoid Arthritis, Systemic Lupus Erythematosus)