- An autoimmune disease
- Unknown etiology
- Genetic factors (represent 15–70% of developing RA)
- Generally presents with arthritis
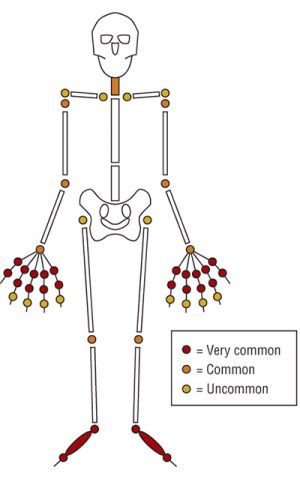
Joints Involvement (Arthritis)
- Usually presents with the insidious onset of pain and stiffness of the small joints of the hands and feet.
- The pain is persistent
- Mainly affects the fingers
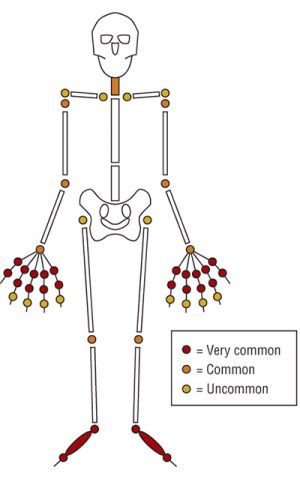
- In 25% of cases RA presents as arthritis of a single joint (e.g. knee): May mimic clinical feature of Lyme disease or a spondyloarthropathy.
- Usually present as polyarthritis:
- Hands: MCP, PIP, DIP joints
- Feet: Ankle, MTP, Tarsal joints (not IP joints),
- Cervical spine (not lumbar spine)
- Wrists
- Elbows
- Knees
- Hip (delayed)
- Shoulder (glenohumeral) joints
- Temporomandibular joints
- Most common chronic inflammatory polyarthritis (affects about 1–2% of the population.
- Expression: Vary from a mild to a most severe debilitating
- More than 10% of patients have a relentless progression and require aggressive drug therapy.
Symptoms
- Usually Insidious onset. Can begin acutely (explosive type)
- Age of Onset
- Any age 10–75 years
- Peak 30–50 years
- Gender
- Female to male ratio = 3:1

- Joint pain
- Worse with waking
- Nocturnal pain interfere with sleep
- Relieved with activity
- Morning stiffness (can last a couple of hours)
- Rest stiffness (e.g. after sitting)
- General:
- Fatigue
- Malaise
- Weakness
- Weight loss
- Disability according to involvement
Signs
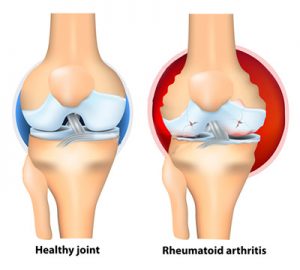
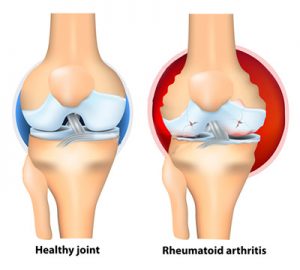
- Effusion and synovial swelling especially of wrist, MCP and PIP joints
- Limited ROM
- Warmth
- Tenderness of joints
- Muscle wasting
- Advanced stage

- Instability
- Deformity (Swan necking, Boutonnière and Z deformities)
- Subluxation: include atlantoaxial subluxation
- Ankylosing
- Impaired a number of everyday functions such as
- Precision grip (using a key or pen)
- Hook grip (carrying a bag)
- Power grip (lifting a jug of water)
Non-Articular Manifestations
- Anemia
- Amyloidosis: mainly kidneys
- Sjögren Syndrome: Dry mouth, Dry eyes
- Vasculitis: Skin Ulcers, Purpura
- Pulmonary Involvement: Pleural Effusion, Fibrosing Alveolitis, Nodules (Caplan Syndrome)
- Cardiac Involvement: Myocarditis, Pericarditis

- Inflammation of the Eyes
- Lymphadenopathy
- Splenomegaly (Felty Syndrome)
- Musculoskeletal Involvement: Bursitis, Subcutaneous Nodules, Bakers Cyst, Tenosynovitis, Carpal Tunnel Syndrome (CTS)
- Peripheral Nerves Involvement: Polyneuropathy, Mononeuritis Multiplex
- Raynaud Phenomenon
Diagnostic Criteria
- Symptom duration more than 6 weeks
- Early morning stiffness more than 1 hour
- Arthritis in three or more regions
- Bilateral tenderness of the metatarsophalangeal (MTP) joints
- Rheumatoid factor (RF) positivity
- Anti-cyclic citrullinated peptide (Anti CCP) antibody positivity
- Symmetry of the areas affected
- Bony erosions evident on radiographs of the hands or Feet (usually in late stages)
- Anemia: Usually normochromic & normocytic
- ESR/CRP: Usually raised according to activity of disease
- Rheumatoid factor
- Positive in about 70–80% (mainly in late disease)
- 15–25% of RA patients will remain negative
- Anti-cyclic citrullinated peptide (anti-CCP) antibodies

- More specific for RA (about 95% specificity)
- X-ray findings:
- Loss of joint space
- Erosion of joint margin: ‘mouse-bitten’ appearance
- Juxta-articular osteoporosis
- Cysts
- Advanced: subluxation or ankylosing
- MRI: Helpful for early diagnosis
- Important Points:
- If the RA factor is positive, it is non-specific, so the anti-CCP antibody should be ordered to confirm the diagnosis.
- RA has a strong cardiovascular risk factor.
Principles
- The patient and family require appropriate reassurance and education support
- Early induction of disease remission is necessary to reduce
- Joint damage
- Malignancy (especially lymphoma)
- Cardiovascular disease
- Due to disease progression in the first 2 years
- Relative aggressive treatment with DMARDs (rather than to start stepwise with analgesics and NSAIDs only) is recommended
- Team approach is highly recommended
- Patient’s functional impairment (home life, work, social activity) should be monitored. Family should be involved in decision making
Advices
- Rest and splinting: For acute flare-up of arthritis

- Exercise
- Especially walking and swimming
- Hydrotherapy in heated pools
- Smoking cessation: Strongly recommended
- Referring to physiotherapists and occupational therapists
- Exercise supervision
- Physical therapy
- Coping in the home and work
- Joint movement
- Daily full range of motion to reduce stiffness
- Diet
- Avoiding animal fats (dairy products and some meats)
- Consumption of fish oil
- Obesity must be avoided
Pharmacological Treatment
- NSAIDS
- Effective but adverse effects are a problem
- Fish Oil

- Corticosteroids
- Oral, Intravenous, Intra articular
- Disease-modifying anti-rheumatic drugs (DMARDs)
- Immunosuppressants
- Azathioprine
- Cyclosporin
- Leflunomide
- Methotrexate
- Cytokine inhibitors (biological DMARDs)
- Anti-TNF α agents: Abatacept, Adalimumab, Etanercept, Infliximab, Golimumab, Rituximab
- Anti-Interleukin-1 agents: Anakinra, Tocilizumab
- Gold Salts
- Others
- Hydroxychloroquine
- Chloroquine
Other Possibilities
- Assistive devices and orthoses (footwear, insoles, cane, walker, wheelchair)
- Orthopedic surgery (joint replacement, synovectomy, plastic hand surgery)
Scroll to top